Pelvic Organ Prolapse
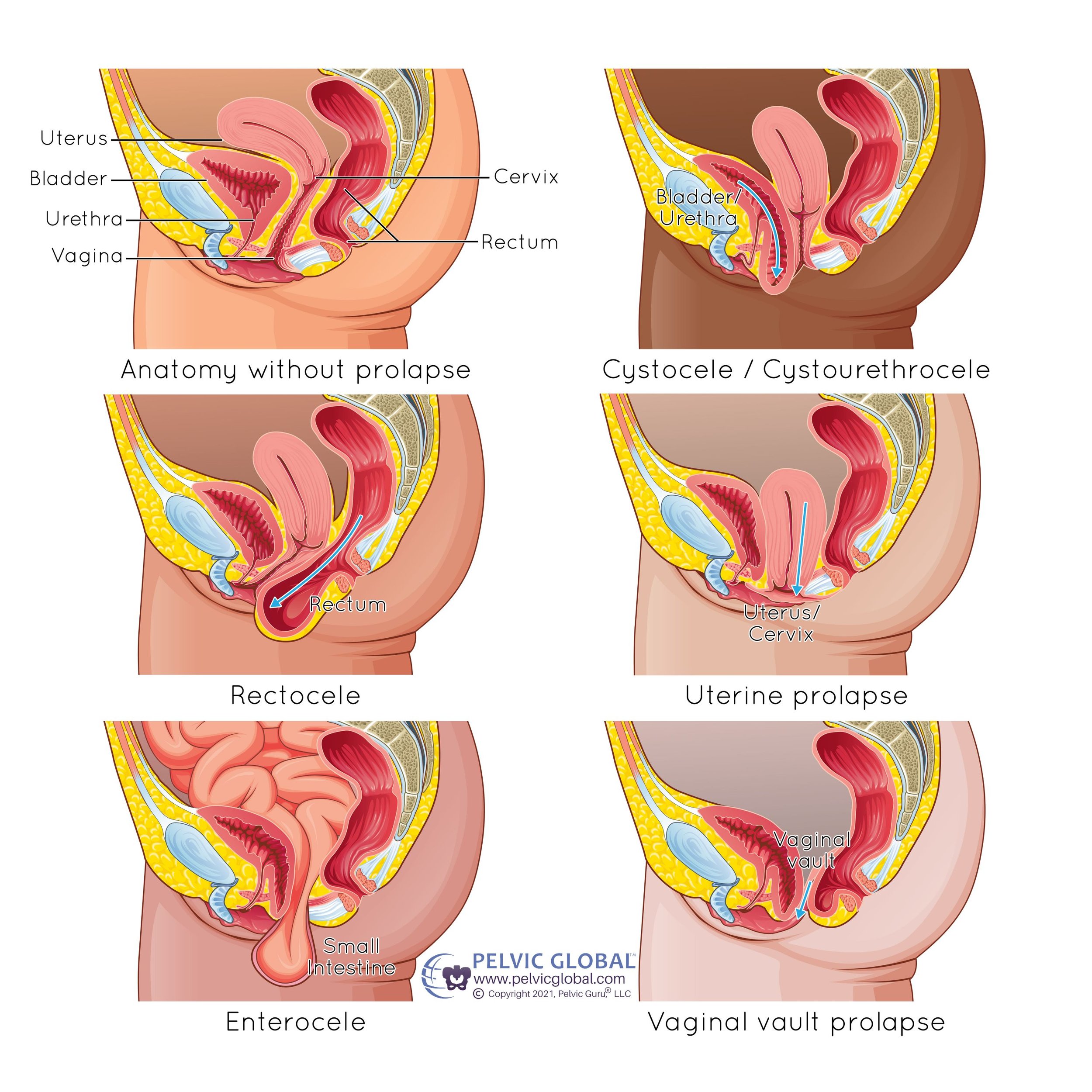
Pelvic organ prolapse (POP) is a common condition that affects many women, particularly those of postmenopausal age. It involves the descent or drooping of one or more pelvic organs (uterus, bladder, rectum, or small bowel) from their normal position into or out of the vagina. This happens when the muscles and ligaments supporting these organs weaken or stretch.
- Pelvic organ prolapse affects over 3 million women in the United States.
- 1 in 9 women will require surgery for their pelvic organ prolapse.
Causes
Several factors contribute to the development of pelvic organ prolapse:
- Childbirth: Vaginal delivery, especially multiple births or large babies, can stretch and weaken the pelvic muscles and tissues, increasing the risk of POP.
- Aging and Menopause: As women age, the decrease in estrogen levels associated with menopause can lead to the weakening of pelvic tissues.
- Obesity: Excess body weight increases pressure on the pelvic floor muscles, contributing to their weakening and possible prolapse.
- Hysterectomy: Removing the uterus can disrupt the support system of the pelvic organs, leading to prolapse.
- Chronic Conditions: Conditions that increase abdominal pressure, such as chronic constipation, chronic cough, or obesity, can increase the risk of developing POP.
- Genetics: Some women may have an inherent weakness in their connective tissue, increasing their risk of prolapse.
Diagnosis
Diagnosing pelvic organ prolapse involves a comprehensive evaluation:
- Medical History: A detailed history helps identify potential risk factors and symptoms related to POP.
- Physical Examination: A pelvic exam is conducted to assess the degree of prolapse and condition of the pelvic floor muscles.
- Post-Void Residual (PVR) Measurement: This test measures the amount of urine left in the bladder after urination, which can help identify other urinary disorders. This can be done with a small ultrasound machine or a catheter.
Treatment Options
Treatment for pelvic organ prolapse aims to relieve symptoms, improve quality of life, and prevent progression. Treatment options range from conservative management to surgical interventions:
Lifestyle Modifications
Lifestyle Modifications
Reducing body weight can decrease abdominal pressure on the pelvic organs.
Avoid heavy lifting and treat constipation to reduce strain on the pelvic floor.
Pelvic Floor Muscle Training
Pelvic Floor Muscle Training
Regularly performing these exercises strengthens the pelvic floor muscles, providing better support for the pelvic organs. Learn More about Kegel Exercises
Please note that if you have chronic pelvic pain, these exercises without guidance from a pelvic floor physical therapist will likely make pain worse.
A specialized physical therapist can help guide a patient through appropriate exercises to help strengthen the pelvic floor. This is more likely to help patients with stage 1 or 2 prolapse and less likely to help when prolapse is at a stage 3 or 4.
Vaginal Pessary for Pelvic Organ Prolapse
A device inserted into the vagina to support the prolapsed organs. Pessaries come in various shapes and sizes and can be fitted to individual patient needs. These can be used short-term while waiting to have surgery or can be used long-term. Patients who use a pessary need regular pelvic exams to monitor the vaginal tissue, typically at least every 3-6 months. Learn more here

Surgical Options
The goal is to restore the normal anatomy of the pelvic organs. This can be performed through the vagina or abdomen, and may involve the use of the patient’s tissues or synthetic materials.
This is a novel surgical device that allows for a less invasive transvaginal approach for pelvic organ prolapse repair. Anchors are passed through the vaginal wall into the sacrospinous ligament to elevate the vagina tissues. Sometimes a concurrent anterior or posterior repair may be performed as well. It can be performed for patients with or without a uterus. While this is a novel device there is currently 4-year data with a 92% success rate.
An anterior repair or anterior colporrhaphy is performed through the vagina to reduce a bulge from the bladder into the vagina.
A posterior repair or posterior colporrhaphy is performed through the vagina to reduce a bulge from the rectum into the vagina.
This is an outpatient surgery that attaches mesh to the front and back of the vagina and then secures this mesh to a ligament over the sacrum (tailbone) to elevate the vagina. It has a very high success rate (90%) and has been used for many years with good success. If a patient still has a uterus, a hysterectomy will need to be performed. Sometimes a concurrent anterior or posterior repair may be performed as well.
This surgery, called a colpocleisis, involves narrowing or closing off the vagina to provide support for prolapsed organs. It is generally reserved for women who no longer wish to have vaginal intercourse. There is a high success rate (over 95%) with this surgery.
Pelvic organ prolapse can significantly impact a woman’s quality of life, but with the right approach, symptoms can be managed effectively and progression can be prevented. Please reach out to the Texas Tech Physicians Urology clinic if you are experiencing symptoms of POP to consult with a provider to explore the most suitable treatment options.